Healthcare Providers
Utah STI Epidemiology
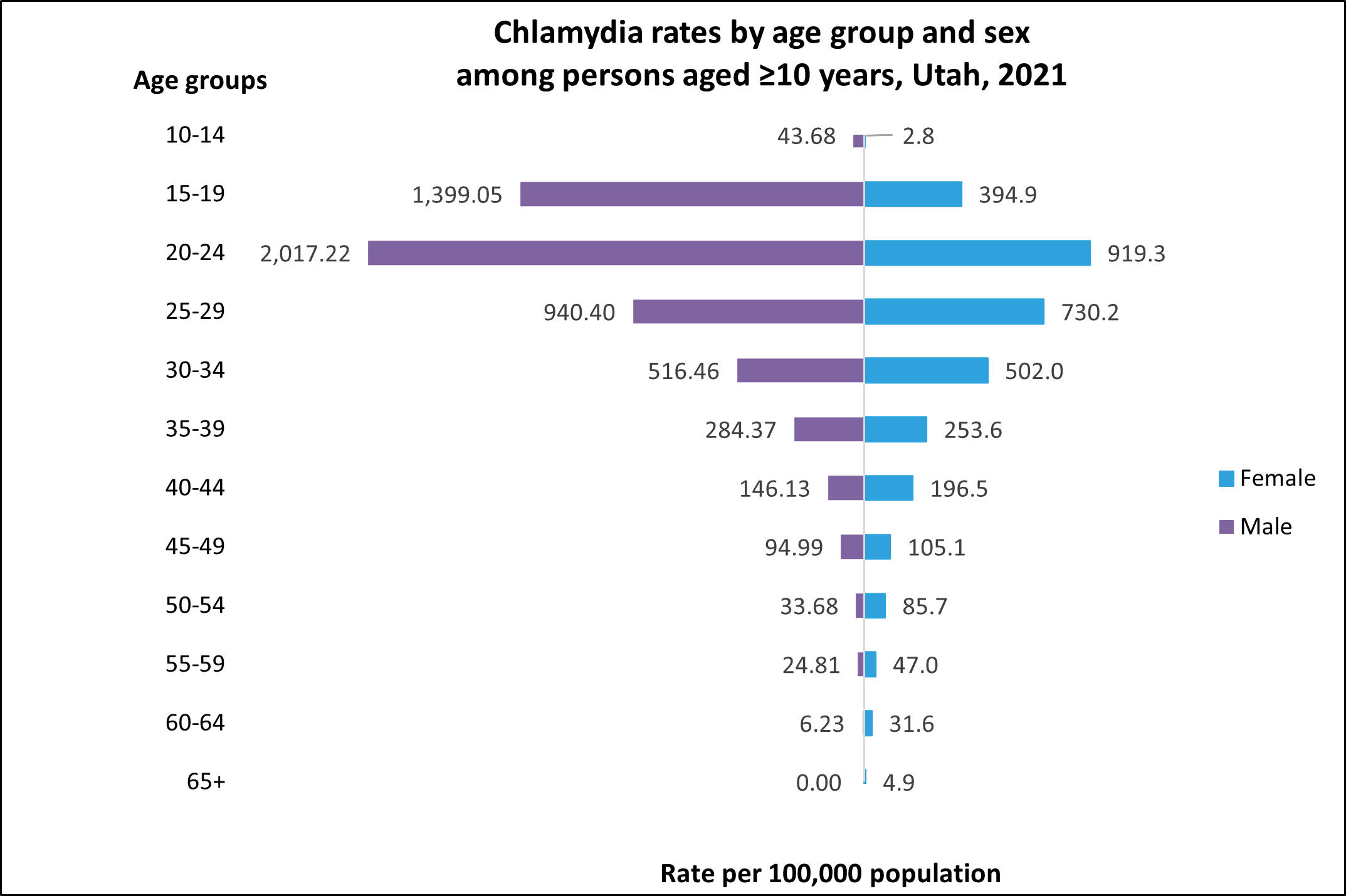
STIs are on the rise throughout the United States and in Utah. In 2020, 2.4 million cases of STIs were reported nationwide and more than half of these cases were among adolescents and young adults ages 15-24.1 Utah is seeing a similar concerning rate of STI cases in adolescents, with 58% of reported chlamydia cases in 2021 occurring in those aged 15-24 years.2
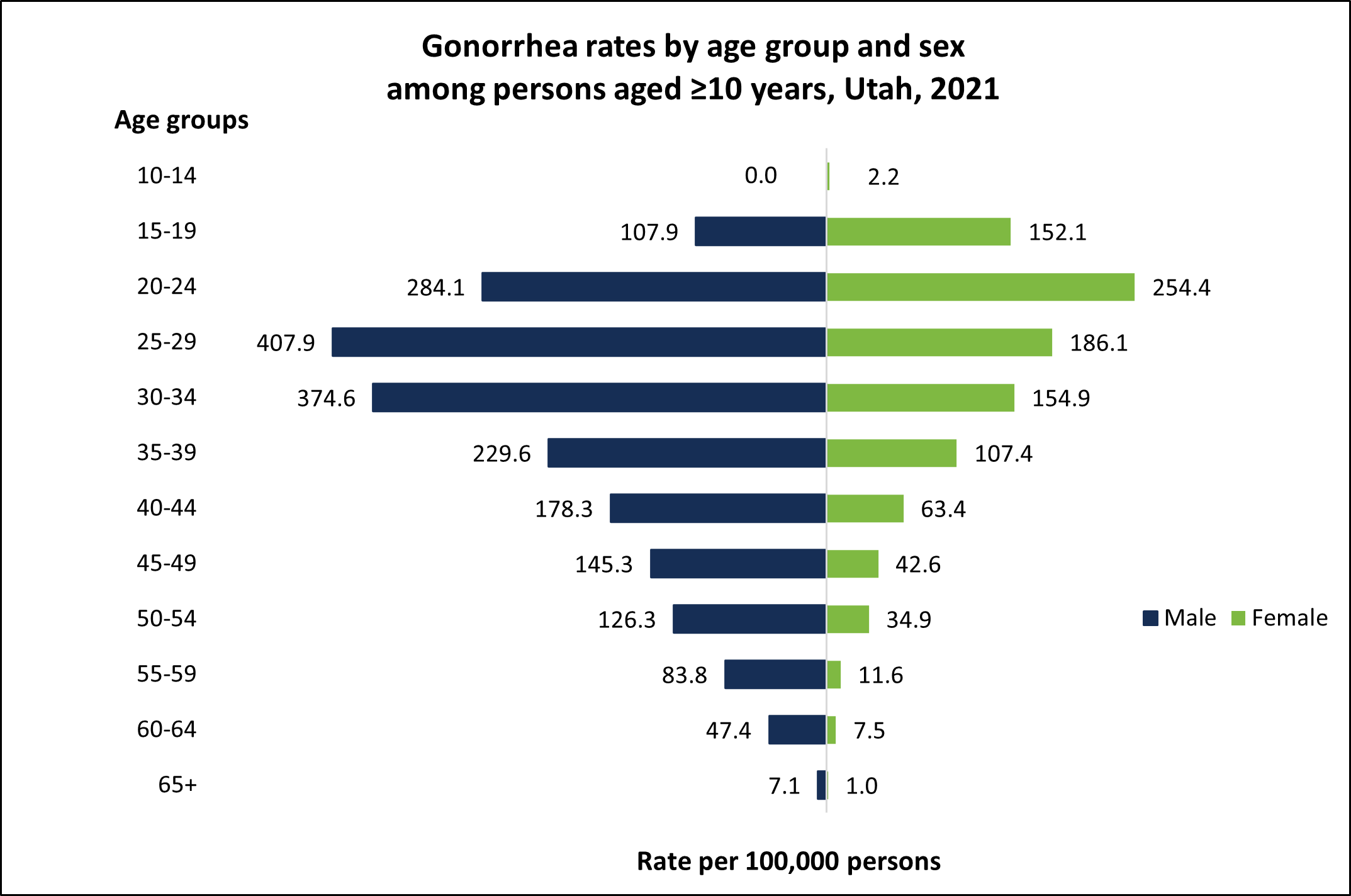
Gonorrhea is also a serious concern. Utah had 3,627 reported cases in 2021, 30% of which were among those ages 15-24.3
What Can Be Done?
As a healthcare provider, you are on the front lines in the fight to curb the spread of STIs. No one said it would be easy, but with the right tactics and information you can make sure your patients know how to stay healthy while being sexually active. Together, we can stop the spread of chlamydia, gonorrhea, and other STIs in Utah. Please see the resources below on STI treatment, screening guidelines, and how to talk to your patients about their sexual history and practices. In addition to these resources, the Utah AIDS Education and Trainer Center Program offers provider-detailing sessions opens in a new tab on STI treatment and screening, PrEP, and taking a sexual health history. Sign up here opens in a new tab.
Treatment
The CDC updated their STI treatment guidelines in 2021 to align with the latest science on the best treatment regimens. Chlamydia and gonorrhea treatment recommendations are listed below, and the full guidelines can be found here: CDC Sexually Transmitted Infection Treatment Guidelines opens in a new tab.
Chlamydia
Doxycycline 100mg orally 2 times/day for 7 days
Azithromycin 1g orally in a single dose is an alternative treatment and can be given to pregnant patients and those with a doxycycline allergy.
Gonorrhea
Ceftriaxone 500mg IM in a single dose for persons weighing <150kg*
* For persons weighing ≥150kg (300lbs), treat with 1g ceftriaxone.
If chlamydia has not been excluded, follow the guidelines above.
Expedited Partner Therapy
Expedited partner therapy (EPT) is an excellent, but underutilized strategy to prevent the spread of STIs which has been legal in Utah since 2009 opens in a new tab. EPT enables providers to treat the sexual partners of patients who are diagnosed with chlamydia or gonorrhea by giving a prescription or medication to the patient to take to their partner without the partner being examined by the prescribing provider. Partners who receive EPT should be given detailed information about their medication and what EPT is. The resources below provide more information for prescribing providers and pharmacists as well as people who receive EPT.
Screening
Due to the high rates of STIs in adolescents, it is imperative to screen sexually active patients regularly. Screening is one of the best tools in our STI prevention toolbox to help slow the spread of STIs and prevent negative health outcomes. Chlamydia, gonorrhea, and syphilis screening guidelines are listed below by population. Routine screening of adolescents who are asymptomatic for certain STIs (e.g., trichomoniasis, bacterial vaginosis, and herpes) is not typically recommended. HIV screening should be discussed and offered to all adolescents.4 The full CDC screening recommendations can be found here: CDC Screening Recommendations opens in a new tab
| Patient Type | Recommendation |
|---|---|
| Adolescent Females | Test sexually active females aged <25 years annually for chlamydia and gonorrhea. Rectal and pharyngeal testing can be considered based on exposure. Retest 3 months after treatment. |
| Pregnant Adolescent Females | Test all pregnant females aged <25 years for chlamydia, gonorrhea, and syphilis at the first prenatal visit. Retest for chlamydia and gonorrhea in the 3rd trimester. Retest for syphilis at 28 weeks and at delivery if at high risk. |
| Adolescent Males Who Have Sex With Males | Test for chlamydia and gonorrhea at all sites of exposure (genital, rectal, pharyngeal) at least annually. Syphilis testing should also be offered annually. More frequent screening can be considered for those at high risk of infection. |
| Adolescent Males Who Have Sex With Females | Testing for chlamydia and gonorrhea can be considered in high prevalence clinical settings (e.g., adolescent services clinics, correctional facilities, etc.). |
| Transgender and Gender Diverse Persons | Screening recommendations should be adapted based on anatomy (i.e., screening recommendations for cisgender women should be extended to transgender men with a cervix). |
Taking a Sexual History
Taking a sexual history is a vital part of routine health care and allows providers to assess and screen patients for a broad range of sexual health concerns. Discussing sexual health offers the opportunity for counseling, education, and sharing information about how to reduce STI risk. The CDC’s guide to taking a sexual history opens in a new tab offers details on how to take a sexual history, including questions to ask your patient. The questions are divided into “the five Ps,” which are topic areas that you should openly discuss with your patients.
The Five Ps
- Partners: Number and gender of your patient's sex partners.
- Practices: What kinds of sex is your patient having?
- Protection from STIs: How does your patient protect themselves?
- Past History of STIs: Has your patient been diagnosed with an STI before?
- Pregnancy Intention: Does your patient desire a pregnancy, and what form of contraceptive are they using?

Teenagers
There are additional considerations to make when you take a teen’s sexual history, particularly surrounding confidentiality as teens are more likely to disclose sensitive information if consent and confidentiality are explained to them. The points below can help providers successfully talk to their adolescent patients about sexual health:5
- Set expectations: speak to the parent and teen together to let them know what to expect, including your intent to speak to the teen privately.
- Respectfully dismiss the parent at an appropriate time so you can speak to the teen alone.
- Reinforce confidentiality: clarify the laws and limits of confidentiality, including when confidentiality may have to be breached, such as in cases of mandatory reporting.
- Avoid assumptions about the teen’s sexual orientation, behaviors, or number of partners.
- Be nonjudgmental and supportive. Using gender-neutral language can help teens feel more comfortable.
- Be concrete and specific with your questions.
- Describe how screening test results will be delivered.

Men Who Have Sex With Men
Men who have sex with men (MSM) might be at increased risk for HIV and STIs because of their sexual network or behavioral or biologic factors. Because of this, providing specific counseling and care is critical, and taking a detailed and comprehensive sexual history is the first step.6 The American Academy of Family Physicians recommends the following:7
- Assess risk during every patient’s first visit, during all comprehensive health assessments, and when evidence suggests a change in behavior.
- Emphasize that the discussion is routine with every patient and remind them that everything is confidential.
- Underscore the importance of needing to know their sexual practices in order to determine appropriate screening and counseling.
- Dispel any concerns about the accessibility of information (such as sexual orientation) to insurers, employers, etc.
- Avoid terms such as gay, queer, and straight when asking about sexual practices or sexual identity.
- Avoid making assumptions about sexual behavior based on age, marital status, disability, or other characteristics.
- Ask specific questions about sexual behavior in a direct, nonjudgmental manner.
Additional Resources
- Utah’s chlamydia & gonorrhea opens in a new tab, and syphilis opens in a new tab report forms can be found on our STI prevention program’s website.
- Provider pocket guides opens in a new tab, MMWR treatment guidelines opens in a new tab, and wall charts opens in a new tab are available online, but if you would like physical copies, please contact the STI program at 801-538-6174. For reportable infections and more information for healthcare providers, please visit our prevention, treatment, and care website opens in a new tab.